What is Personalised Care?
Personalised care represents a new relationship between people, professionals and the system. It happens when we make the most of the expertise, capacity and potential of people, families and communities.
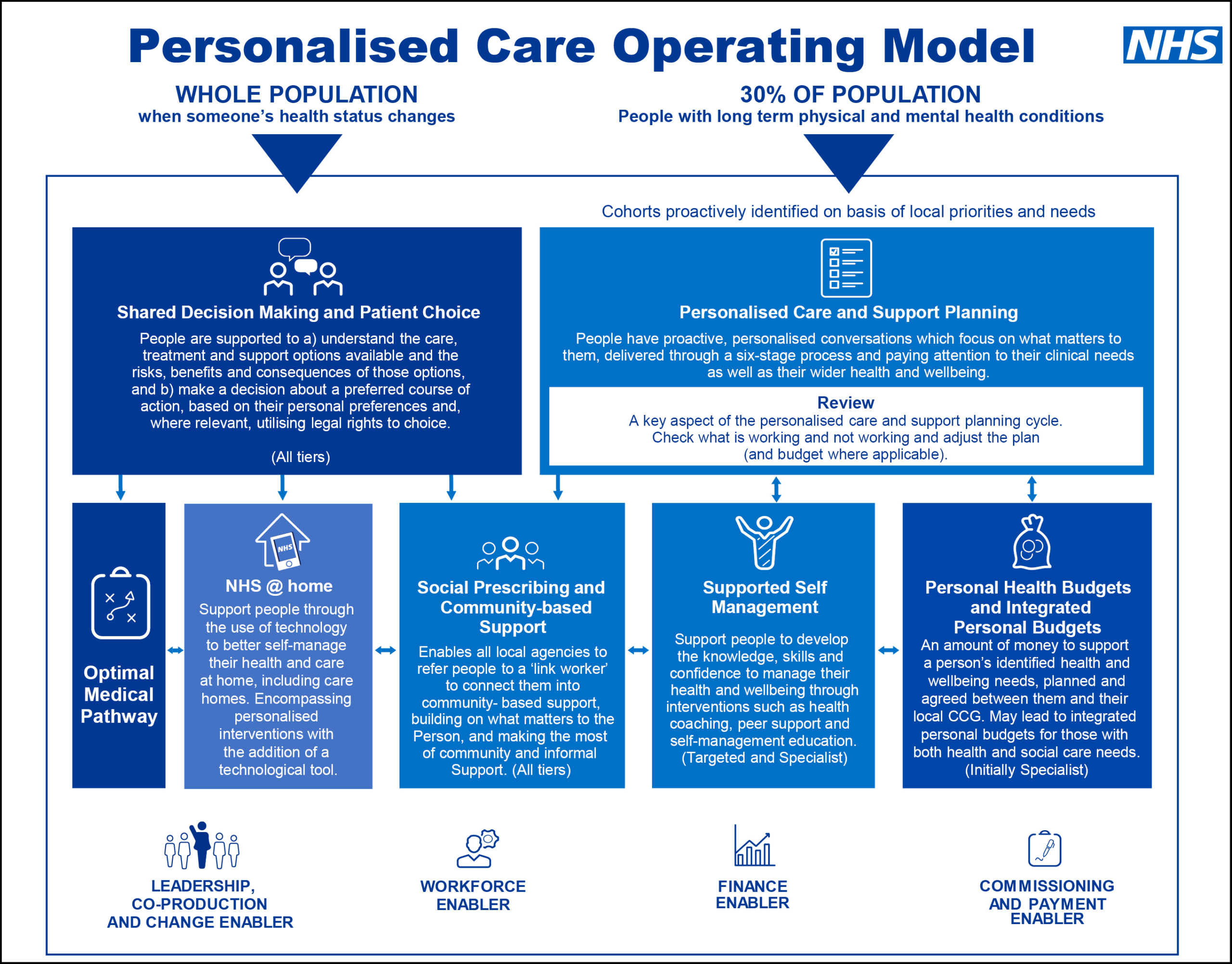
Personalised care means people have choice and control over the way their care is planned and delivered, based on ‘what matters’ to them and their individual strengths and needs. The NHS Long Term Plan published in January 2019 has a commitment to personalised care.
This short animation explains what personalised care means for people, professionals and the health and care system.